It’s been almost a year since Lesley was diagnosed with breast cancer. Last November, Lesley felt an abnormal bump on her breast and went to her family doctor to get it checked out. She was soon sent to a neighbouring hospital to get tests done and the results came back as urgent.
“My daughter-in-law works at Markham Stouffville Hospital (MSH), part of Oak Valley Health, and mentioned the Breast Health Centre (BHC) there,” said Lesley. “I went on their website, downloaded a referral form, and took it to my family doctor to start my process.”
By the next day, Lesley had an appointment set up and a list of tests to be done.
“I was met with a fantastic team that was so professional, friendly, and informative.”
The team includes pathologists, family physicians, nurses, mammography technologists, radiologists, ultrasound technologists, surgeons, social workers, and volunteers trained in the needs associated with our patients. A newer role was also added to the team to optimize the patient’s care right from the initial referral and throughout the treatment journey for our patients. The nurse navigator act as an accessible point-person to clarify care plans, and support patients by care coordination across the different interdisciplinary health team.
On January 6, 2021, Lesley went into surgery for a lumpectomy (partial mastectomy) with Dr. Crystal Pallister, a general surgeon at MSH who focuses on breast, thyroid, and colon cancer. “I just can’t believe how comfortable I felt going into the hospital during COVID-19 knowing I was being completely protected. Before my surgery Dr. Pallister was so reassuring and all of the nurses helped calm my nerves.”
Surgery was a success and the health care team was pleasantly surprised how well Lesley’s surgery looked.
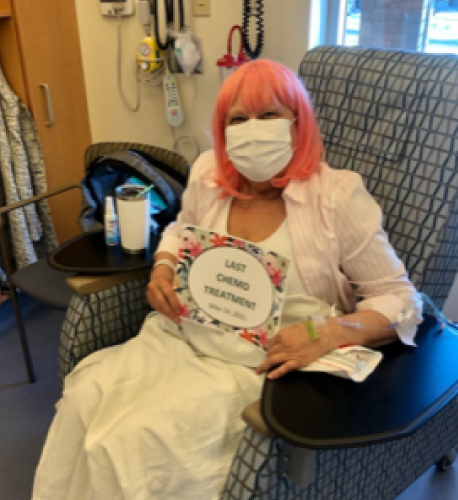
Although surgery removed the cancerous invasive tumour, the team recommended Lesley undergo chemotherapy to increase the success rate.
“The oncology nurses explained everything about my chemotherapy treatment, what to expect, and answered all my questions. The team spent about an hour with my daughter and I. We couldn’t believe the amount of information we were given and the number of support groups available for patients and caregivers.”
Lesley was given a phone number for 24-hour care during her chemotherapy. “You are hoping you won’t need to call the line but I did and the team was great. They even called to follow-up to see how I was doing.”
Lesley noted that the oncology nurses and Dr. Mateya Trinkaus, an oncologist at MSH, were so compassionate during each appointment and they made sure to answer all of her questions about her physical and mental health.
“There was no question unanswered by the team at MSH. They gave me so much information that I felt prepared to make my own decisions. They didn’t make the decisions for me – they gave me the tools to feel comfortable making them myself.”
Lesley says what stands out to her the most is the compassion in which the entire team treated her. “They treated me like I was a part of their family. A lot of times you feel like you’re just a number, but for someone to say your name, say hello, and acknowledge you – that makes all the difference.”
The BHC at MSH is a model of patient-centred care, meaning the health system revolves around the patient. If you require assessment or treatment at the BHC, rest assured we have the most advanced screening tools and an expert team of health specialists. We deliver “one-stop” coordinated care in a setting built for your comfort and privacy.
MSH participates in clinical trials to help provide treatment options to our patients. Clinical trials are research studies that involve people. Through clinical trials, doctors find new ways to improve treatments and the quality of life for people with disease. For more information about oncology clinical trials please speak with your medical oncologist or visit the Office of Research page for information about active trials.
